Surgical options
Bariatric surgery isn’t a magic fix, but rather, can be seen as a tool to use in your health improvement journey. Surgery can be an extremely helpful tool to overcome biological pathways; working at a biochemical and hormonal level to facilitate weight loss. But it is also important to address social, behavioural and environmental factors for long term success.
The terms weight loss surgery, bariatric surgery and metabolic surgery are used interchangeably. Bariatric surgery is a major procedure and, for most, a life altering event that helps achieve better health, reduce chronic disease and improve overall quality of life.

Surgery intentionally alters your gastrointestinal tract, removing part of your stomach and/or re-routing your intestines to change your biology. Bariatric surgery works by a number of mechanisms including the following:
- Decreasing your stomach size – All forms of bariatric surgery reduce the volume of your stomach which reduces appetite and makes you feel full quicker.
- Gut hormone changes – All forms of bariatric surgery alter gut hormones and biology. Appetite is reduced and glucose and calorie regulation significantly altered. Hormone signals to your brain are altered.
- Reducing calorie absorption – Some bariatric operations reduce the amount of the intestine that is exposed to food and this results in varying degrees of malabsorption.
Northland Health & Weight offers three surgeries: Laparoscopic Sleeve Gastrectomy, Laparoscopic Gastric Bypass and Laparoscopic One Anastomosis Gastric Bypass. It is important to educate yourself about the different surgeries so you can discuss with the surgeon the best option for you.
Laparoscopic Sleeve Gastrectomy
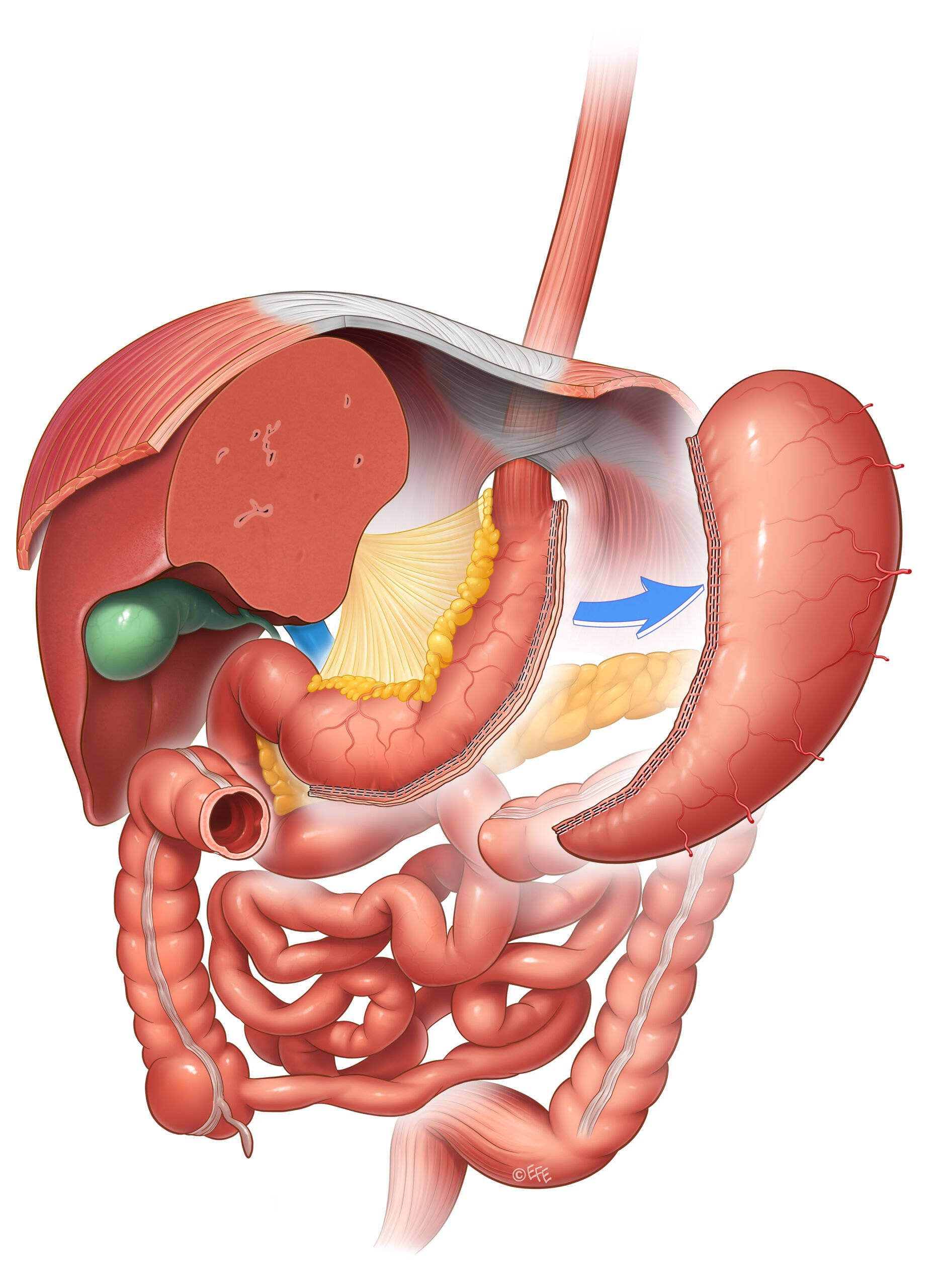
© Dr Levent Efe, courtesy of IFSO
A Sleeve Gastrectomy converts the stomach from the shape of a bag to the shape and size of a banana. A stapling device is used to remove greater than 2/3rds of the stomach. There are no changes to your intestines. When you eat, food passes through the normal route, although this is now much smaller.
Most people lose weight quite quickly over the first year following sleeve surgery. You will generally reach your lowest weight after 12-18 months after surgery. On average, people lose 25-30% of their body weight, but this does vary.
Laparoscopic Gastric Bypass
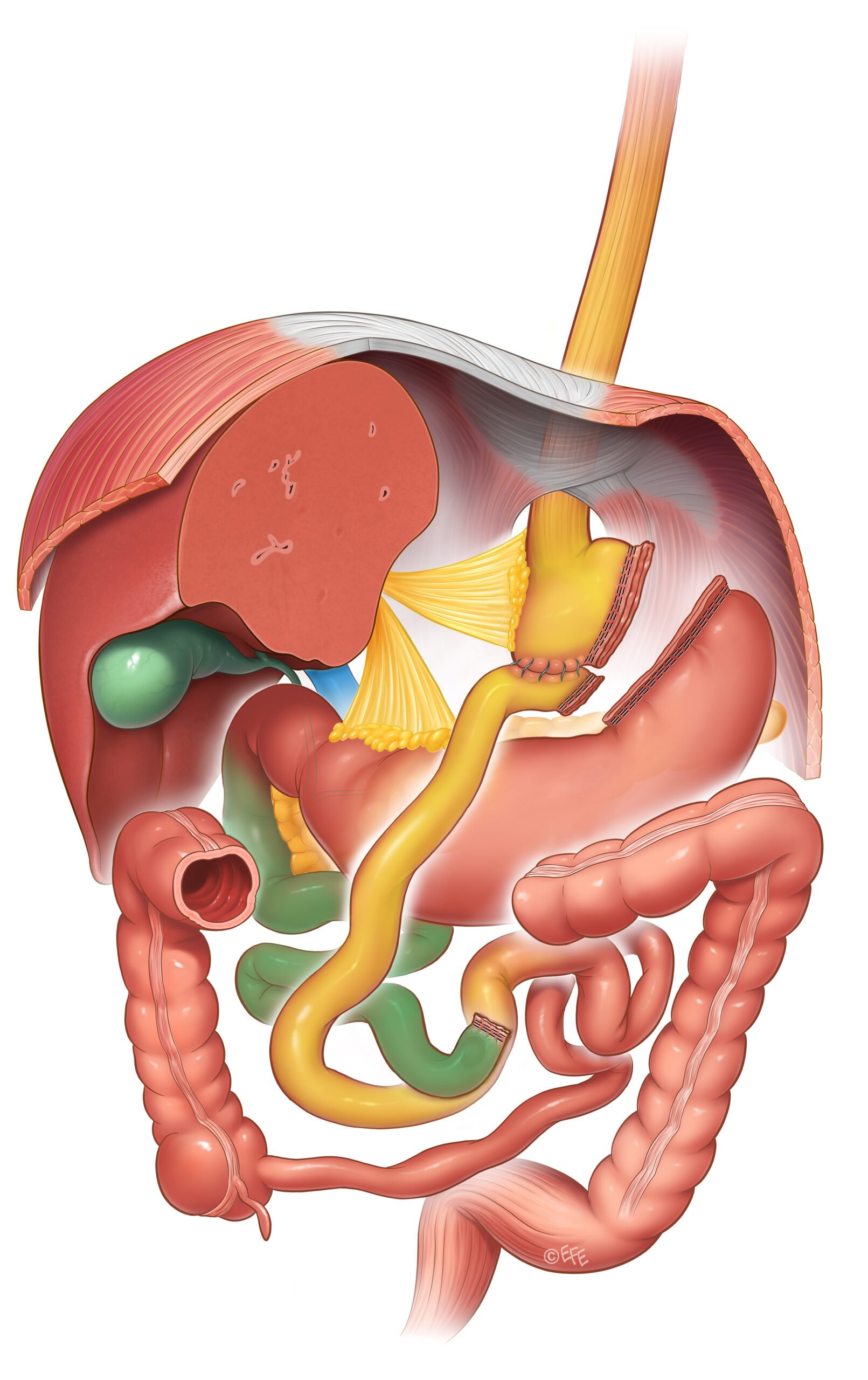
© Dr Levent Efe, courtesy of IFSO
Gastric Bypass, also known as a Roux-en Y Bypass, has been used for 60 years or more. However, it’s a bit more of an involved operation. The very top part of your stomach is made into a small pouch and separated from the remaining 80% of your stomach. This pouch is about the size of a large egg. The intestines are divided, rearranged and connected to this new stomach pouch. When you eat and drink, food comes down your oesophagus, into the stomach pouch and then directly into your intestines. The rest of the stomach, liver and pancreas are bypassed but not removed. These secretions and digestive fluids drain into the intestines downstream.
Most people lose weight quite quickly over the first year following bypass surgery. You will generally reach your lowest weight after 12-18 months after surgery. On average, people lose 30-35% of their body weight, but this does vary.
Laparoscopic One Anastomosis Gastric Bypass
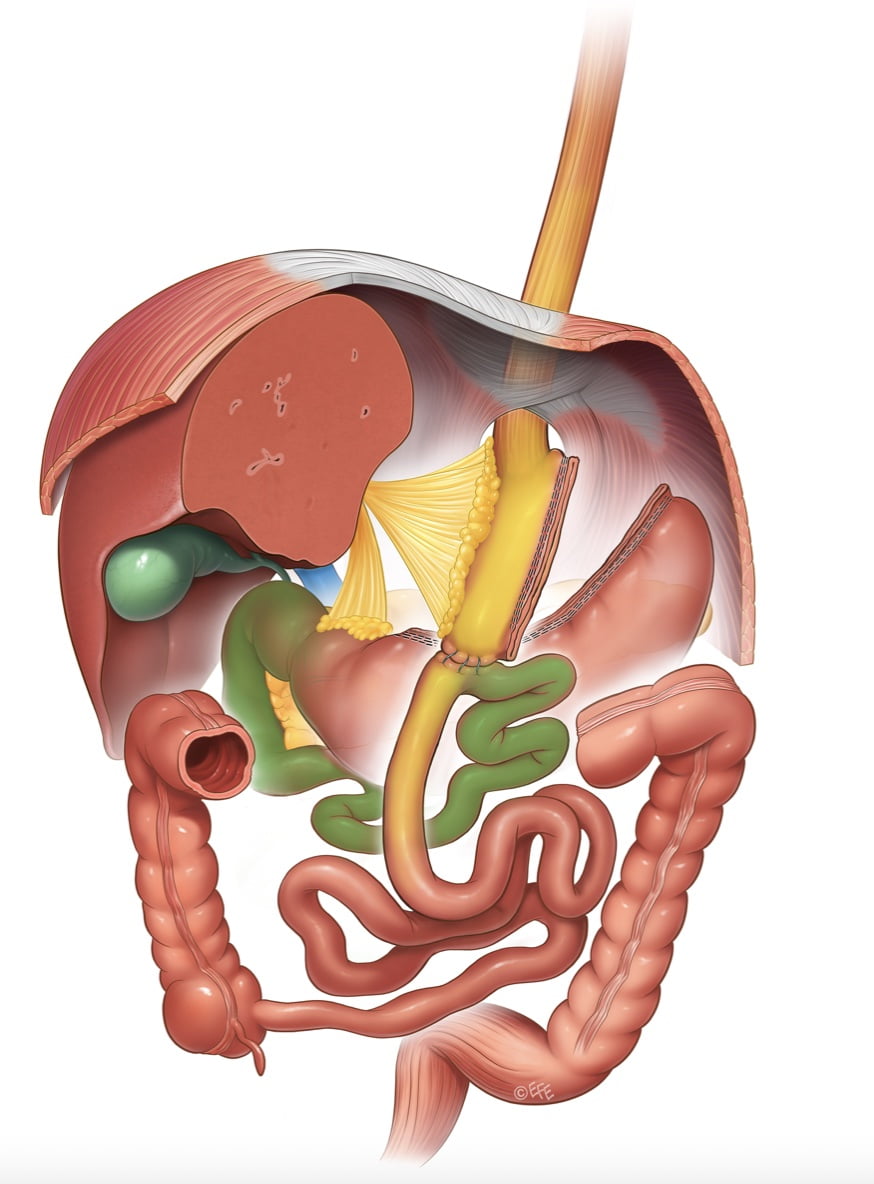
© Dr Levent Efe, courtesy of IFSO
One Anastomosis Gastric Bypass, also known as a Mini Gastric Bypass or Single Anastomosis Gastric Bypass, is a modification on the standard Roux-en-Y Gastric Bypass. It is slightly quicker to perform and involves one less bowel join so has become a popular choice in recent times. The top part of your stomach is made into a small tube (slightly longer than a standard bypass) and separated from the remaining 70% of your stomach. A loop of intestine is then brought up and connected to this new stomach pouch. When you eat and drink, food comes down your oesophagus, into the stomach tube and then directly into your intestines. The rest of the stomach, bile drainage and pancreas are bypassed but not removed. Secretions and digestive fluids from theses organs follow their usually pathway.
You will generally reach your lowest weight 12-18 months after surgery. On average, people lose 30-35% of their body weight, but there is variation in the amount of weight that people lose following surgery.
Which operation is right for me?
There is no straightforward answer to this question. You may have an idea of the procedure you would prefer. This may be based on your own research or from talking to other people who have had surgery. The options will be discussed and it will be a joint decision between you and your surgeon.
More information about bariatric operations can be found at:
Is surgery right for me?
The American Society for Metabolic and Bariatric Surgery (ASMBS) and the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) are two international societies dedicated to the field of Bariatric Surgery. Updated guidelines were published in 2022 – ‘Indications for Metabolic and Bariatric Surgery.’ Bariatric surgery is a major change with significant health benefit, but also has risks and long term implications. This guideline recommends surgery be considered for the following people:
- BMI ≥ 35 kg/m2
- BMI ≥ 30 kg/m2 for those with an obesity-related health condition
It is important to remember that bariatric surgery needs to performed safely and some medical conditions mean surgery is not possible. In addition, lifestyle change prior to surgery is important to improve long term outcomes.
Surgical outcomes
On average people who have bariatric surgery lose about 25-35% of their starting weight. It is important to note that bariatric surgery may not make you a ‘normal’ weight, but the weight loss is substantial and sustained. Therefore, we encourage you to consider that your ‘best weight’ is one where your health and quality of life is improved and sustained.
Significant health improvements are seen in obesity related illnesses such as diabetes, sleep apnoea, fatty liver, high blood pressure and many more. Joint pain and mobility are greatly improved and people can often be active in ways that previously were not possible. There are also improvements is energy, vitality, mental health and sleep.
Risks
Bariatric surgery should be considered irreversible. It is a permanent rearrangement of your gastrointestinal system to facilitate major weight loss and improve your health. And it’s not without risk.
There are the risks that are common to all surgery such as issues with the anaesthetic, infection, blood clots and even a very small but real risk of death.
Early on after surgery there is a 1-2% chance of major bleeding or leakage from the staple lines and bowel joins. This may require repeat surgery and can complicate recovery significantly. If this was to occur, it usually does so in the first few days to weeks after surgery.
In the long term, nutritional supplementation is required lifelong to prevent major deficiencies. Tweaking may be required with time. Stomach ulcers can occur and anti-inflammatory medication and smoking need to be avoided to minimize this risk. The risk of gallstone formation is increased due to the weight loss.
Specific risks by operation:
Laparoscopic Sleeve Gastrectomy
- The chance of acid reflux/heartburn is increased after a sleeve. This is usually balanced out by weight loss, and if it occurs, is often controlled by acid lowering medication. However, over time this can become difficult to manage for some and occasionally additional surgery is required.
- A twist or a narrowing in the sleeve can occur with time. This usually results in hard to control acid reflux/heartburn.
- Weight recurrence can be an issue if healthy eating habits aren’t adhered to.
Laparoscopic Gastric Bypass
- An ulcer at the join between stomach and intestine (called a marginal ulcer) can occur. This is often associated with smoking and NSAID pain relief.
- A bowel obstruction called an internal hernia can occur as a result of the intestines being re-routed. If this was to occur, surgery is required.
- You may experience dumping syndrome, a condition experienced by 70-80% of people who have had a gastric bypass. If you eat too much sugar, fat or alcohol, or large amounts of food, the stomach rapidly empties into the small intestine leading to blood sugar and fluid abnormalities. It is not considered a health risk but can be very unpleasant. You can avoid dumping syndrome if you follow the recommended diet after surgery.

