Preparation for surgery
Preparing for change
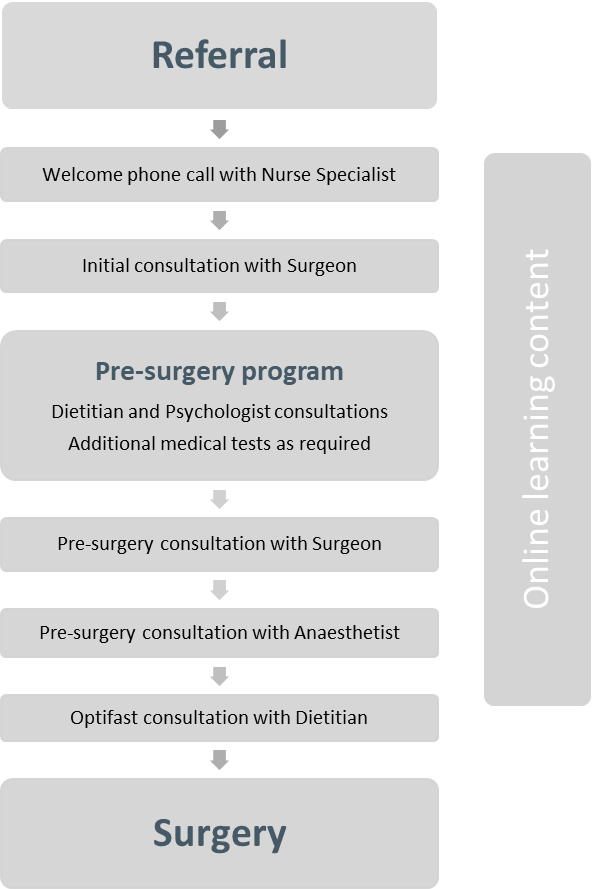
As with any elective surgery, it is important to get prepared. The operation is only one part of your weight loss and health improvement journey. Our specialist team will aim to support you for several months to make changes and form habits for long-term success. This will be individually tailored to your needs. We can also offer appointments to suit you (in person or where appropriate virtually via zoom or phone). Further medical investigations may be required and will be arranged as needed. We believe it is important to invest the time required during this phase so that you have the tools required for a good long-term outcome.
Exercise
During the lead up to surgery we ask that you commit to a form of exercise. Over time, the sort of activity you will be able to do may change but investing time to have the exercise habit formed is an important step. Aim for dedicated physical activity 3-4 times per week, 30-45min on each occasion. Resistance exercises are important to maintain muscle mass. Exercise may not make a big difference on the scales, but it has numerous non-weight related health benefits.
Pre-surgery surgeon consultation
Once you are ready for surgery, an appointment will be arranged with your surgeon. The specific surgery plan, risks and benefits will be discussed. A surgical date will be planned and a pre-surgery consultation with our anaesthetist arranged.
Optifast®
In the weeks prior to your surgery, you will be prescribed a liquid diet (Intensive Level of the Optifast® VLCD™ program). This provides less than 800 calories per day and leads to mild ketosis, decreasing your appetite and promoting further weight loss of between 1kg and 2.5kg per week. This reduces the amount of fat on your liver to make the surgery safer and easier, as well as easier for you to transition to a fluid diet after surgery.
Hospital admission
The Northland Health & Weight team will provide you an intended operation date and an Optifast® start date well in advance. Your operation will take place at Kensington Hospital, Whangārei. Hospital staff will contact you during the week or two prior to confirm your pre-operative instructions and re-discuss medication changes. There may be additional blood tests.

We highly recommend you arrange an appointment in advance with your GP in the week or two prior to surgery just to touch base. They are an invaluable resource in your journey.
You will be admitted to hospital in the morning of your surgery. From the admission area, you will be taken to the pre-operative area to change into a hospital gown and get an IV line. It is here that you will be seen by the surgeon and anaesthetist. When the operating room is ready, you will be taken through. You will be connected to monitors, have a breathing mask fitted and then be put to sleep.
You will wake up in the recovery unit with monitoring attached to you. You will stay in recovery under the care of a recovery nurse until you are awake, stable and comfortable. Then, you will be transferred to the ward. You will be drowsy and probably sleep on and off for a few hours.
On the Ward
On the ward you will be cared for by a specialist nursing team. You will be reviewed daily by the surgeon and anaesthetist. The hospital stay is usually two days. You will be able to drink water in small amounts immediately after surgery. Your oral intake will be increased to a liquid diet over your hospital stay. Early mobilisation is important in recovery, and we encourage you to spend as much time in a chair as you are able and to walk the hallway frequently. Medication will initially be administered intravenously but this will transition to oral formulations within 24 hours.
Discharge
You are suitable to go home day two if:
- Your pain is controlled
- You are off supplemental oxygen
- You are tolerating oral liquids enough to maintain hydration (usually 1500ml/day)
You will be given a plan for your usual medication and a prescription will be provided for the medicines required in the recovery period. Your wounds will have temporary waterproof dressings on them to allow for showering.
After surgery
There is a 6-8 week period of dietary progression after surgery from liquids to normal food, accepting that your new ‘normal’ changes. Your dietitian will provide you information on this phase prior to surgery.
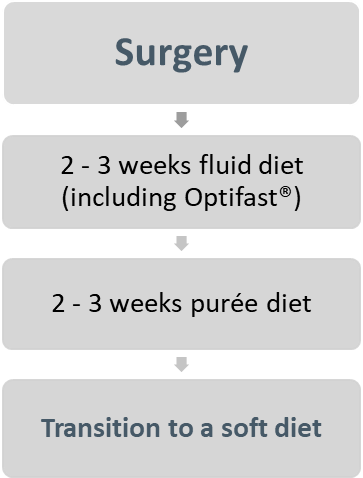
Multivitamins are required for life after bariatric surgery and our team will provide the details on these prior to surgery. These should be bariatric surgery specific and there are a number of reputable online suppliers. We recommend sourcing these prior to surgery and they can usually begin in the purée diet phase.
Return to work
Although your abdomen will feel comfortable within a week or two, people often find they are quiet fatigued during the first 3-4 weeks. It is for this reason that we generally recommend taking a month off work after surgery and then if you feel up to it, you may choose to return early.
Activity
It is important to get back to 30 minutes a day of cardio exercise, such as brisk walking, as soon after surgery as possible. We do not recommend heavy lifting or strenuous activity for 4- 6 weeks after the surgery. You will be able to start exercising at the gym 6 weeks after the operation.
Follow up
Our Nurse Specialist will schedule a phone call with you a week after surgery. The team at Northland Health & Weight will also follow you for two years after your operation, most intensely within the first six months. There will be nurse, dietitian, psychologist and surgeon appointments and, where possible, these can be held virtually over the phone or via Zoom. Lab work is required at 3 months, 6 months, 12 months and annually thereafter. At the appropriate time, we will hand over your ongoing medical care to your primary care team (GP clinic).
Your new life
Bariatric surgery, and the preparation required, is an amazing opportunity for change. Although it is not designed to fix every issue in your life, a lot of people describe it as a major life event where they have had a ‘reset’. The weight loss outcomes are significant, but we encourage you to focus on the non-scale victories and make these your most valued post-surgery change. These include: improved fitness levels, engagement in activities with family, improved self-confidence, less medications and improved chronic health conditions (and many more).
However, it’s not all smooth sailing. Surgery is a permanent change to your gastrointestinal system, designed to improve your health. People report big changes post-surgery, which can be challenging (things like excess skin, hair loss, relationship difficulties) and rewarding. We cannot predict what challenges might show up for you post-surgery, but what we can predict is that we will be here to support you as required.

